More than 10 Hip Replacement Risks and Complications
(50,000 metal hip replacement patients RECALLED to hospital for X-rays over toxic fears
THOUSANDS of patients with ‘metal on metal’ hips are being recalled for tests after experts revealed they could be toxic.
http://www.express.co.uk/life-style/health/822810/metal-hip-replacement-xray-blood-test-toxic-sepsis-risk
By OLIVIA LERCHE PUBLISHED: 08:24, Fri, Jun 30, 2017 | UPDATED: 08:48, Fri, Jun 30, 2017 – SEE Second Part below)
In hip replacement risks are similar to those associated with all joint replacements such as Vein thrombosis, dislocation, loosening, 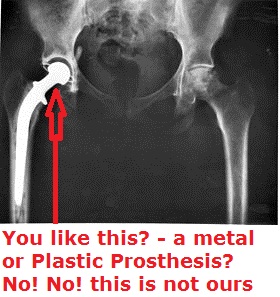
impingement, infection, osteolysis, metal sensitivity, nerve palsy, pain and death.
Vein thrombosis
Venous thrombosis such as deep vein thrombosis and pulmonary embolism are relatively common following hip replacement surgery.
Dislocation
Dislocation is the most common complication of hip replacement surgery. At surgery the femoral head is taken out of the socket, hip implants are placed and the hip put back into proper position. It takes eight to twelve weeks for the soft tissues injured or cut during surgery to heal. During this period, the hip ball can come out of the socket. The chance of this is diminished if less tissue is cut, if the tissue cut is repaired and if large diameter head balls are used. Surgeons who perform more of the operations each year tend to have fewer patients dislocate. Doing the surgery from an anterior approach seems to lower dislocation rates when small diameter heads are used, but the benefit has not been shown when compared to modern posterior incisions with the use of larger diameter heads. Patients can decrease the risk further by keeping the leg out of certain positions during the first few months after surgery. Use of alcohol by patients during this early period is also associated with an increased rate of dislocation.
Fracture
Bones with internal fixation devices in situ are at risk of periprosthetic fractures at the end of the implant, an area of relative mechanical stress. Post-operative femoral fractures are graded by the Vancouver classification.
Osteolysis
Many long-term problems with hip replacements are the result of osteolysis. This is the loss of bone caused by the body’s reaction to polyethylene wear debris, fine bits of plastic that come off the cup liner over time. An inflammatory process causes bone resorption that may lead to subsequent loosening of the hip implants and even fractures in the bone around the implants. In an attempt to eliminate the generation of wear particles, ceramic bearing surfaces are being used in the hope that they will have less wear and less osteolysis with better long-term results. Metal cup liners joined with metal heads (metal-on-metal hip arthroplasty) were also developed for similar reasons. In the lab these show excellent wear characteristics and benefit from a different mode of lubrication. At the same time that these two bearing surfaces were being developed, highly cross linked polyethylene plastic liners were also developed. The greater cross linking significantly reduces the amount of plastic wear debris given off over time. The newer ceramic and metal prostheses do not always have the long-term track record of established metal on poly bearings. Ceramic pieces can break leading to catastrophic failure. This occurs in about 2% of the implants placed. They may also cause an audible, high pitched squeaking noise with activity. Metal-on-metal arthroplasty releases metal debris into the body raising concerns about the potential dangers of these accumulating over time. Highly cross linked polyethylene is not as strong as regular polyethylene. These plastic liners can crack or break free of the metal shell that holds them.
Loosening
As shown on right radiography, hip prosthesis displays aseptic loosening (arrows) 
On the radiography, it is normal to see thin radiolucent areas of less than 2 mm around hip prosthesis components, or between a cement mantle and bone. However, these may still indicate loosening of the prosthesis if they are new or changing, and areas greater than 2 mm may be harmless if they are stable. In the first year after insertion of uncemented femoral stems, it is normal to have mild subsidence (less than 10 mm).
Metal sensitivity
Concerns are being raised about the metal sensitivity and potential dangers of metal particulate debris. New publications have demonstrated development of pseudotumors, soft tissue masses containing necrotic tissue, around the hip joint. It appears these masses are more common in women and these patients show a higher level of iron in the blood. The cause is unknown and is probably multifactorial. There may be a toxic reaction to an excess of particulate metal wear debris or a hypersensitivity reaction to a normal amount of metal debris.Metal hypersensitivity is a well-established phenomenon and is common, affecting about 10–15% of the population. Contact with metals can cause immune reactions such as skin hives, eczema, redness and itching. Although little is known about the short- and long-term pharmacodynamics and bioavailability of circulating metal degradation products in vivo, there have been many reports of immunologic type responses temporally associated with implantation of metal components. Individual case reports link hypersensitivity immune reactions with adverse performance of metallic clinical cardiovascular, orthopedic and plastic surgical and dental implants.
Metal toxicity
Most hip replacements consist of cobalt and chromium alloys, or titanium. Stainless steel is no longer used. All implants release their constituent ions into the blood. Typically these are excreted in the urine, but in certain individuals the ions can accumulate in the body. In implants which involve metal-on-metal contact, microscopic fragments of cobalt and chromium can be absorbed into the patient’s bloodstream. There are reports of cobalt toxicity with hip replacement patients.
Nerve palsy
Post operative sciatic nerve palsy is another possible complication. The incidence of this complication is low. Femoral nerve palsy is another but much more rare complication. Both of these will typically resolve over time, but the healing process is slow. Patients with pre-existing nerve injury are at greater risk of experiencing this complication and are also slower to recover.
Chronic pain
A few patients who have had a hip replacement suffer chronic pain after the surgery. Groin pain can develop if the muscle that raises the hip (iliopsoas) rubs against the edge of the acetabular cup. Bursitis can develop at the trochanter where a surgical scar crosses the bone, or if the femoral component used pushes the leg out to the side too far. Also some patients can experience pain in cold or damp weather. Incision made in the front of the hip (anterior approach) can cut a nerve running down the thigh leading to numbness in the thigh and occasionally chronic pain at the point where the nerve was cut (a neuroma).
Death
The rate of death for elective hip replacements is significantly less than 1%.
Leg length inequality
The leg can be lengthened or shortened during surgery. Unequal legs are the most common complaint by patients after surgery with over lengthening the most common problem. Sometimes the leg seems long immediately after surgery when in fact both are equal length. An arthritic hip can develop contractures that make the leg behave as if it is short. When these are relieved with replacement surgery and normal motion and function are restored, the body feels that the limb is now longer than it was. If the legs are truly equal, the sense of inequality resolves within a month or two of surgery. If the leg is unequal, it will not. A shoe lift for the short leg, or in extreme cases, a corrective operation may be needed.
Metal-on-metal hip implant failure
Failures may relate to release of minute metallic particles or metal ions from wear of the implants, causing pain and disability severe enough to require revision surgery in 1–3% of patients. Design deficits of some prosthesis models, especially with heat-treated alloys and a lack of special surgical experience accounts for most of the failures. The cause of these failures remain controversial, and may include both design factors, technique factors, and factors related to patient immune responses (allergy type reactions). It is not clear to what extent this phenomenon negatively affects orthopedic patients. However, for patients presenting with signs of an allergic reactions, evaluation for sensitivity should be conducted. There is increasing awareness of the phenomenon of metal sensitivity and many surgeons now take this into account when planning which implant is optimal for each patient.
50,000 metal hip replacement patients RECALLED to hospital for X-rays over toxic fears
THOUSANDS of patients with ‘metal on metal’ hips are being recalled for tests after experts revealed they could be toxic.
http://www.express.co.uk/life-style/health/822810/metal-hip-replacement-xray-blood-test-toxic-sepsis-risk
By OLIVIA LERCHE
PUBLISHED: 08:24, Fri, Jun 30, 2017 | UPDATED: 08:48, Fri, Jun 30, 2017
All patients with the devices are being urged to have checks by medical professionals after a safety warning was issued by a health watchdog.
The Medicines and Healthcare products Regulatory Agency (MHRA) said the move is a precautionary measure.
There have been concerns in the past over the devices – with a limited number of patients previously being recalled for tests. But now the issue could be even more serious than first believed.
Now experts have said people could be at risk of muscle or bone damage – and even high levels of metal in the blood.
Blood poisoning – also known as sepsis is a life-threatening condition.
The Medicines and Healthcare products Regulatory Agency (MHRA) as a precautionary measure has today issued updated guidance for healthcare professionals who manage patients implanted with metal-on-metal hip replacements.
This updated guidance replaces the previous advice provided in 2012.
The key changes include additional recommendations regarding monitoring patients and are designed to ensure longer term followup is undertaken for all patients with these implants.
Dr McGuire added: “The clinical advice we have received indicates patients will likely have the best outcomes if these problems are detected early, monitored and treated if necessary.
“If you have any questions about your hip replacement, speak with your GP or implanting surgeon.”
A hip replacement is a common type of surgery where a damaged hip joint is replaced with an artificial one.
Adults of any age can be considered for a hip replacement, although most are carried out on people between the ages of 60 and 80.
blob:http://www.express.co.uk/d6251f36-cd91-474d-b334-5d7e16bc453e